- Reduced semen motility, abnormal morphology leading causes of male infertility in regions, researchers find
- Recommend general body cleansing, detoxification few months before conception
Researchers in Nigeria and South Africa have raised the alarm on decreasing trend in quality of sperm in men from the two countries.
The researchers in a study titled “Trends in semen parameters of infertile men in South Africa and Nigeria” and published, last week, in the journal Scientific Reports found: “Our findings provide a quantitative evidence of an alarming decreasing trend in semen parameters in Nigeria and South Africa from 2010 to 2019. It also proves that astheno- and teratozoospermia are the leading causes of male infertility in these regions.
“In addition to this, it also shows empirically that semen parameters decrease with advancement in age. These findings are the first report of temporal trends in semen parameters in Sub-Saharan countries, necessitating a thorough investigation on the underlying factors promoting this worrisome decline.”
Asthenozoospermia (or asthenospermia) is the medical term for reduced sperm motility, while teratospermia or teratozoospermia is a condition characterized by the presence of sperm with abnormal morphology that affects fertility in males.
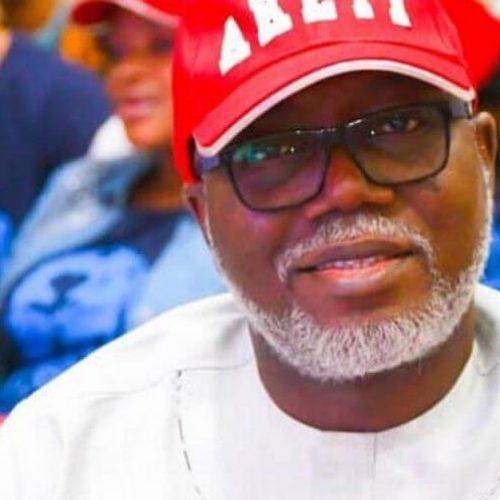
The researchers led by the joint pioneer of In Vitro Fertilisation (IVF) in Nigeria, President, African Fertility Society (AFS), Prof. Oladapo Adenrele Ashiru, and Medical Director of Medical Art Center (MART), Ikeja, Lagos, Nigeria, include: Edidiong Nnamso Akang from the Department of Anatomy, College of Medicine, University of Lagos, Idi-Araba, Lagos, Nigeria and Section of Infectious Diseases, Department of Internal Medicine, Yale School of Medicine, Yale University, New Haven, Connecticut, United States of America (USA); Chinyerum Sylvia Opuwari of the Department of Medical Biosciences, Faculty of Natural Sciences, University of the Western Cape, Bellville, South Africa; Swesme Enyioma‑Alozie of the Department of Anatomy, Baze University, Abuja, Nigeria; Lionel Wildy Moungala of Androcryos Andrology Laboratory, Johannesburg, South Africa; Tamarapreye Emmanuel Amatu and Ibrahim Wada of Nisa Premier Hospital, Abuja, Nigeria; Rose Ogeyi Ogbeche and Oluwatoyin Omolayo Ajayi of The Bridge Clinic, Lagos, Nigeria; Mojisola Modupe Aderonmu and Olaitan Boluwatife Shote of Medical Art Centre (MART), Ikeja, Lagos, Nigeria; Lateef Adekunle Akinola of the Department of Obstetrics and Gynaecology, Medison Specialist Women’s Hospital, Lagos, Nigeria; and Ralf Henkel of the Department of Metabolism, Digestion and Reproduction, Imperial College London, London, United Kingdom (UK).
The researchers noted: “There are conflicting reports on trends of semen parameters from different parts of the globe. However, in recent times there is dearth of information on the trend in Sub-Saharan countries.
Therefore, in this study we aimed at determining the trends in semen parameters in Nigeria and South Africa between 2010 and 2019. It is a retrospective study of semen analyses of 17,292 men attending fertility hospitals in Nigeria and South Africa in 2010, 2015 and 2019. Excluded from the study are patients who had undergone vasectomy and those who had a pH less than five or greater than 10.
A vasectomy (male sterilisation) is a surgical procedure to cut or seal the tubes that carry a man’s sperm to permanently prevent pregnancy. It is usually carried out under local anaesthetic, where one is awake but doesn’t feel any pain, and takes about 15 minutes.

The following variables were assessed: ejaculate volume, sperm concentration, progressive motility, total progressively motile sperm count (TPMSC), total sperm count, and normal sperm morphology.
“Between 2010 and 2019, significant trends of decreasing values were observed in normal sperm morphology, and the ejaculatory volume, indicating a progressive deterioration of the values in both countries. In Nigeria, there were significant decreases in progressive motility, TPMSC, and sperm morphology between 2010 and 2019.
“Spearman’s rank correlation revealed significant negative associations between age and morphology, progressive motility, and TPMSC. Patients in South Africa were younger than those from Nigeria, with also a significantly higher sperm morphology, sperm concentration, progressive motility, total sperm count and TPMSC.”
Semen parameters including sperm concentration, total sperm count, sperm motility, TPMSC, sperm morphology, and semen volume are essential diagnostic tools for assessing the reproductive health and fertility status of men.
Several studies have revealed conflicting results on the trend of semen parameters postulating there are no temporal trends and if there are then they are region dependent. However, a decline has been observed since the late 1930s in western countries including the United States, Australia, and Europe.
Aberrations in sperm parameters remain the leading cause of male factor infertility. Between 1965 and 2015, Sengupta et al. reported an over 32 per cent reduction in sperm concentration among European men. From the most populous countries in Asia, Adiga et al., reported 22.92 per cent, 30.3 per cent and 51.25 per cent decrease in sperm motility, sperm count, and morphology respectively among Indian men.
Similarly, significant decline in sperm concentration and total sperm count has been reported among 327,373 Chinese men within four decades. From South America, a 23-year (1995–2018) study in Brazil also reported decline in sperm parameters. Another study reported an overall 73 per cent decline in sperm concentration in African men over a period of 50 years (1965–2015).
Globally, the declining trend in semen parameters seem to be more consistent. However, in recent times there is paucity of information on the trends of semen parameters in Sub-Saharan African countries. This makes it difficult to ascertain the enormity of the burden of male factor infertility in African families.
This is a retrospective study that included the semen analysis reports of 17,292 men attending fertility hospitals in Nigeria and South Africa in 2010, 2015 and 2019. All patients who had undergone vasectomy and those who had pH less than five or greater than 10 were excluded from this study. Data from Nigeria were recorded from four hospitals: Medical ART Center, Maryland, Lagos; Bridge Clinic, Ikeja, Lagos; The Medison Hospital, Lekki, Lagos; Nisa Premier, Jabi, Abuja. While those from South Africa were recorded from patients attending Androcryos Andrology Laboratory, Johannesburg; Ampath Andrology Laboratory, Pretoria; and Lancet Andrology Laboratory, Pretoria.
Semen was collected by masturbation into a sterile plastic container after two to seven days of abstinence and examined within one hour after liquefaction in accordance with the 2010 World Health Organisation (WHO) guidelines. The following variables were assessed: ejaculate volume, sperm concentration, progressive motility, TPMSC, total sperm count, and normal sperm morphology.
All data were calculated using the MedCalc® statistical software (Ver. 20.118; MedCalc Software Ltd, Ostend, Belgium). Data was tested for normal distribution using the Chi-squared test. Since data was not normally distributed, non-parametric tests were performed. Mann Whitney test was used to compare cumulative data between Nigeria and South Africa, whereas the Kruskal–Wallis test was used to compare differences between the different years of data retrieval (2010, 2015, and 2019). Dunn’s post-hoc analysis was carried out on samples that showed any significant difference of, total sperm count, TPMSC, and volume was noted for South Africa, with a significant increase in progressive motility (P TPMSC and volume, while progressive motility increased in South Africa. In addition, normal morphology, progressive motility, TPMSC decreased significantly, while sperm concentration, total sperm count, and semen volume remained unchanged in Nigeria.
Furthermore, a declining trend was only noted for normal morphology, progressive motility, and TPMSC. The combined data of both countries showed a significant decrease in normal morphology, progressive motility, TPMSC and semen volume.
Similarly, a significant declining trend was observed for normal morphology, progressive motility, TPMSC and semen volume in the combined date.
Over the years, as observed from 2010 to 2019, significant trends of decreasing values are observed for, sperm concentration (−0.23 per cent), normal sperm morphology (−50 per cent), total sperm count (−1.1 per cent) and ejaculatory volume (−7.4 per cent) indicating a progressive deterioration of the values, combining data from Nigeria and South Africa. Due to the small data from South Africa in 2019 on progressive motility and TPMSC, a combined assessment of both countries was not done.
In addition, some changes were noted in the trends for Nigeria and South Africa between 2010 and 2019. In Nigeria, a decline was observed in sperm concentration (−13 per cent), progressive motility (−86.8 per cent), and TPMSC (−77.9 per cent), with an increase in total sperm count (2.2 per cent), while there were no changes observed for morphology, and ejaculatory volume.
In South Africa, a decline in sperm concentration (−7.4 per cent), normal sperm morphology (−55 per cent), total sperm count (−0.1 per cent), and ejaculatory volume (−13.8 per cent) was observed. Data for progressive motility and TPMSC is not available for South Africa due to small sample size.
Spearman`s rank correlation for abstinence and age with semen parameters from Nigeria and South Africa showed weak associations between the duration of abstinence and all semen parameters, whereas there were moderate negative correlations between age and morphology was detected.
Separate analysis for South Africa and Nigeria resulted in significant overall fits of the model, but only a significantly fitting model for Nigeria and not for South Africa. While the impact of age was just significant for the South African cohort, no significant impact of the independent variables was observed. For teratozoospermia, the model for the combined data from South Africa and Nigeria was significant with good goodness of fit. However, in the separate analysis, the model was only significant for Nigeria with the ejaculate volume having a significant impact.
The researchers concluded: “This study reports observations of a rapid decreasing trend in semen parameters among men visiting fertility clinics in South Africa and Nigeria between 2010 and 2019. This alarming increase in astheno- and teratozoospermia is the leading cause of male infertility in Nigeria and South Africa respectively. This study also identifies ageing as a factor associated with the decreased semen parameters.
“Our findings may give some insight into the temporal trends in semen parameters specifically in Sub–Sahara Africa and suggest further studies to investigate the other causes of the increasing male factor infertility. Furthermore, trends of semen parameters in different regions of the world need to be investigated, causes identified and solutions proffered for this increasing problem challenging men`s reproductive health.”
On the possible causes of the decline in sperm quality, Ashiru blamed sexually transmitted diseases, which has been on the rise, especially Chlamydia and gonorrhoea. He also implicated the use of recreational drugs, alcohol, smoking and other substances.
The fertility expert said there is now increase use of laptops, iPads and tablets as well as mobile phones, which contain heavy metals such if cobalt generate heat of the male reproductive system when put on the lap. “Causing significant decrease in sperm. This should be avoided,” he said.
Ashiru said also identified environmental toxins and occupational hazards. He said prominent in this group are petrochemicals, oil fossils as in the Niger- Delta area, the paint industry, and pesticides.
He said climate change; tight underwear and exposure to extreme heat are capable of decreasing sperm count. Ashiru said other endocrine disruptors are present in artificial foods, artificial sweeteners and Genetically Modified Organism (GMO) food products.
On the solution to rising male infertility in Nigeria and South Africa, Ashiru said: “The solutions rest in avoiding many of the toxins, and as it now being recommended. If one is thinking of conception, it is good to treat the body to a general body cleansing and detoxification at least two to three months before the process. It would help remove heavy metals, toxic chemicals and more from the body.”
Source: TheGuardian